Rn cognition dementia and delirium 3.0 case study test – Introducing the RN Cognition, Dementia, and Delirium 3.0 case study test, an invaluable resource for nurses navigating the complexities of cognitive impairment. This test provides a comprehensive framework for understanding, assessing, and managing these conditions, empowering nurses to deliver exceptional care to their patients.
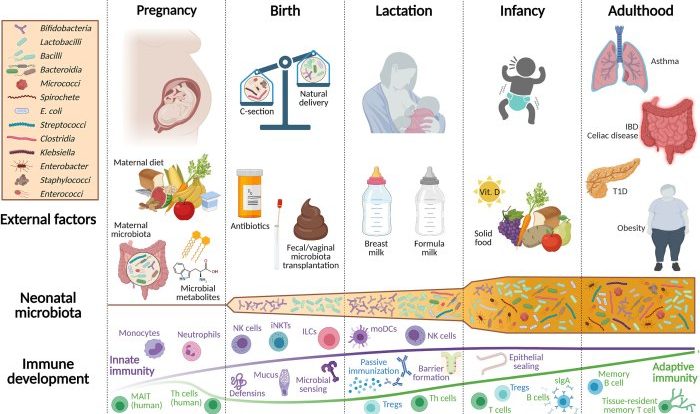
With a focus on the latest research and evidence-based practices, this test delves into the multifaceted nature of cognitive impairment, dementia, and delirium. It explores the role of the nurse in identifying, evaluating, and intervening to promote optimal patient outcomes.
Definition and Overview

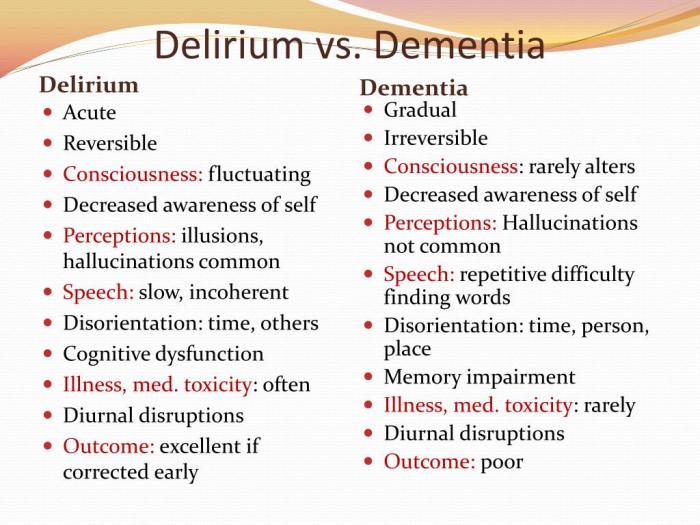
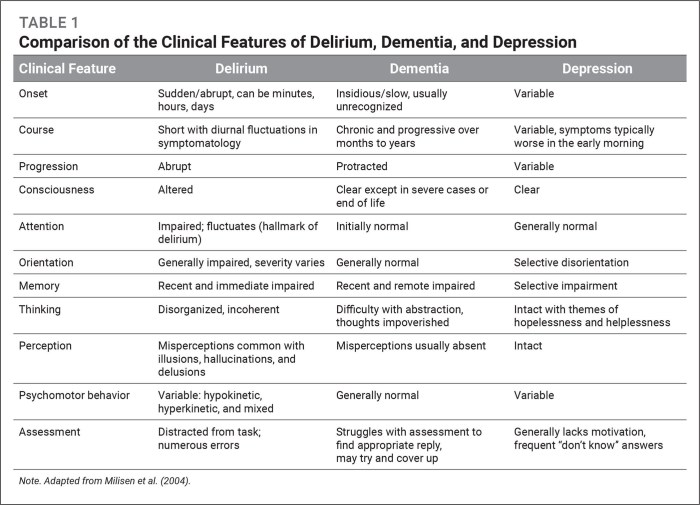
RN cognitionrefers to the cognitive abilities and processes of registered nurses, including their ability to think, remember, and make decisions. Dementiais a general term for a decline in cognitive function that affects memory, thinking, and behavior. Deliriumis a sudden and severe change in cognitive function that is often caused by an underlying medical condition.
Cognitive impairment, dementia, and delirium are common conditions in the healthcare setting, affecting a significant proportion of older adults. These conditions can have a profound impact on patients’ quality of life, as well as on the healthcare system.
Assessment and Evaluation
The RN plays a crucial role in assessing and evaluating patients for cognitive impairment, dementia, and delirium. This involves:
- Observing the patient’s behavior and interactions
- Conducting cognitive screening tests
- Reviewing the patient’s medical history and current medications
- Interviewing family members and other caregivers
Specific assessment tools and techniques used by nurses include:
- Mini-Mental State Examination (MMSE)
- Montreal Cognitive Assessment (MoCA)
- Clock Drawing Test
- Functional Activities Questionnaire (FAQ)
Management and Interventions
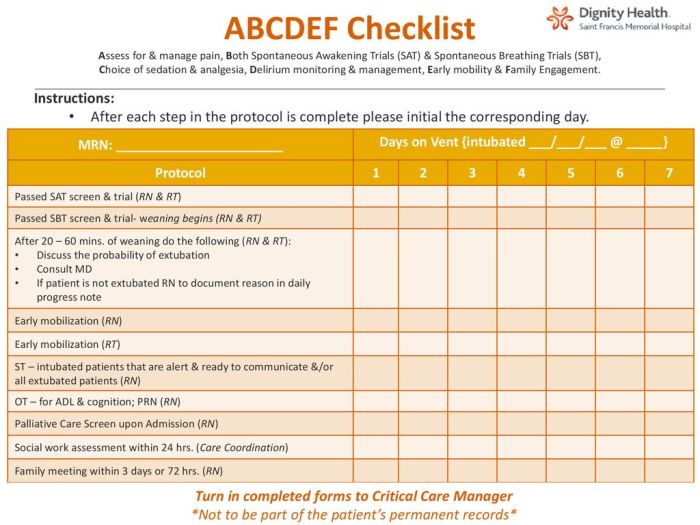
The management of cognitive impairment, dementia, and delirium requires a comprehensive approach that involves:
- Creating a safe and supportive environment
- Providing cognitive stimulation and reality orientation therapies
- Managing behavioral symptoms
- Collaborating with other healthcare professionals
Creating a safe and supportive environment includes providing the patient with a familiar and structured routine, minimizing environmental stressors, and ensuring that the patient has access to appropriate assistive devices.
Cognitive stimulation and reality orientation therapies are designed to improve the patient’s cognitive function and orientation to reality. These therapies may involve activities such as reminiscence therapy, music therapy, and art therapy.
Case Study Analysis
A 78-year-old woman is admitted to the hospital with a sudden onset of confusion and agitation. She is disoriented to time and place, and she is unable to recall recent events. She has a history of hypertension and diabetes, and she is currently taking several medications, including a diuretic and an antihypertensive.
The nurse assesses the patient using the MMSE and finds that she scores a 12 out of 30. The nurse also interviews the patient’s family members, who report that she has been increasingly forgetful and confused over the past few months.
The nurse suspects that the patient is experiencing delirium, which is likely caused by a urinary tract infection. The nurse initiates treatment for the infection and provides the patient with a safe and supportive environment. The patient’s symptoms improve over the next few days, and she is discharged home with instructions to follow up with her primary care physician.
Collaboration and Communication: Rn Cognition Dementia And Delirium 3.0 Case Study Test
Collaboration among healthcare professionals is essential in caring for patients with cognitive impairment, dementia, and delirium. This includes:
- Communicating with family members and other caregivers
- Participating in interdisciplinary team meetings
- Developing and implementing care plans
RNs play a key role in communicating with family members and other caregivers about the patient’s condition and care plan. They can also provide support and education to family members and caregivers, who are often the primary providers of care for patients with cognitive impairment.
Interdisciplinary team meetings are an important forum for discussing the patient’s condition and care plan. These meetings typically involve nurses, physicians, social workers, and other healthcare professionals who are involved in the patient’s care.
Commonly Asked Questions
What is the prevalence of cognitive impairment, dementia, and delirium in healthcare settings?
Cognitive impairment, dementia, and delirium are highly prevalent in healthcare settings, affecting a significant proportion of older adults. Studies indicate that up to 80% of nursing home residents may experience some form of cognitive impairment.
How does the RN Cognition, Dementia, and Delirium 3.0 case study test help nurses?
The test provides nurses with a structured approach to assessing, evaluating, and managing patients with cognitive impairment, dementia, and delirium. It guides nurses in recognizing symptoms, selecting appropriate assessment tools, and implementing evidence-based interventions.
What is the role of collaboration in caring for patients with cognitive challenges?
Collaboration among healthcare professionals, including nurses, physicians, social workers, and family members, is crucial in providing comprehensive care for patients with cognitive challenges. By sharing expertise and perspectives, the team can develop individualized care plans that address the patient’s physical, cognitive, and emotional needs.